 PITUITARY ADENOMAS
PITUITARY ADENOMAS
5. Treatment
*5.1 Medical Treatment
Prolactinoma
A Prolactinoma remains a medically treated tumor first option.
The principle is to use the inhibitory action of Dopamine via dopaminergic receptors located on the surface of PRL secreting cells. Inhibition leads to diminution of production and decrease in storage vesicles and thus decrease in tumor volume. The action is cytostatic.
Dopamine agonists came into use in the late 1970s with Parlodel® (Bromocriptine, daily intake).
The second generation is represented by Norprolac® (Quinagolide, daily intake) and the third since the early 2000s by Dostinex® (Cabergoline, weekly or daily intake).
Dostinex® is currently the treatment of choice, except in pregnancy, because it is more effective and better tolerated than other dopamine agonists.
Side effects of these agonists are: low blood pressure, digestive disorders with nausea, vomiting, especially at the beginning of treatment. It is currently recommended to do an annual cardiac echography because of the occurrence of valvulopathies.
The anti-secretory and anti-tumor effect is rapid, within a few weeks, with a drop in the PRL and a decrease of more than 50% of the tumor volume (Figure 7). However, cytostatic medical treatment should be continued at least until menopause. Weaning can be attempted after at least 3 years off hypersecretion and with normal MRI. Recurrence does not occur in 20-30% of patients 11,17. True resistance to dopamine agonists is rare between 5 and 10% 78.
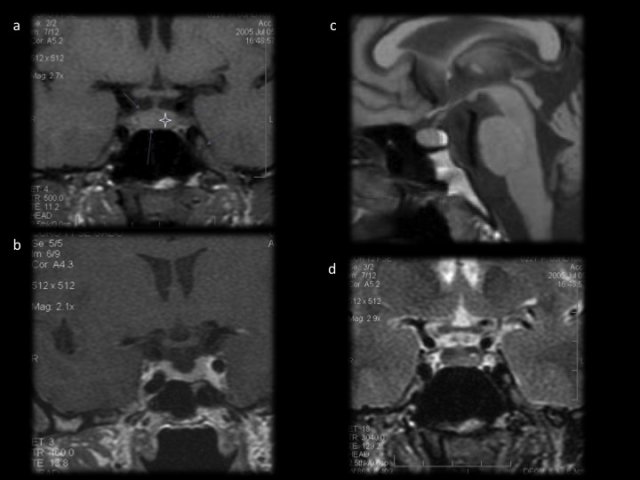
- Figure 7 : a : séquence T1 coronale sans gadolinium ; b : séquence T1 avec gadolinium, l’antéhypophyse se réhausse de façon homogène. c : en sagittal, la posthypophyse apparaît en hypersignal sur les séquences en T1 sans gadolinium. d : Image d’une hypophyse normale en T2 coronale. Les veines caverneuses sont parfaitement visibles.
Particularities of pregnancy:![]() For microadenomas or "small" macroadenomas not in close proximity to the chiasm, fertility is restored in 90% with the decline of the hyperprolactinemia. In case of pregnancy, Parlodel is the preferred drug of choice because of its many years in use, but no teratogenic effects have been observed for cabergoline(Lebbe Clin Endo 2010)41
For microadenomas or "small" macroadenomas not in close proximity to the chiasm, fertility is restored in 90% with the decline of the hyperprolactinemia. In case of pregnancy, Parlodel is the preferred drug of choice because of its many years in use, but no teratogenic effects have been observed for cabergoline(Lebbe Clin Endo 2010)41 ![]() The risk of increase in tumor volume is very low (<2%) and it can be stopped during pregnancy without any specific follow up protocol (no PRL assay due to the physiological increase during pregnancy), and breastfeeding is allowed. Laboratory tests and an MRI should be done during the waning.
The risk of increase in tumor volume is very low (<2%) and it can be stopped during pregnancy without any specific follow up protocol (no PRL assay due to the physiological increase during pregnancy), and breastfeeding is allowed. Laboratory tests and an MRI should be done during the waning. ![]() For macroadenomas, the risk of increase in tumor volume justifies the continuation of medical treatment during pregnancy. Follow up will include visual assessment every trimester and an MRI if signs of mass effect (compression). Breastfeeding is contra-indicated.
For macroadenomas, the risk of increase in tumor volume justifies the continuation of medical treatment during pregnancy. Follow up will include visual assessment every trimester and an MRI if signs of mass effect (compression). Breastfeeding is contra-indicated.![]() The algorithm in Figure 14 summarizes the current management of prolactinomas.
The algorithm in Figure 14 summarizes the current management of prolactinomas.
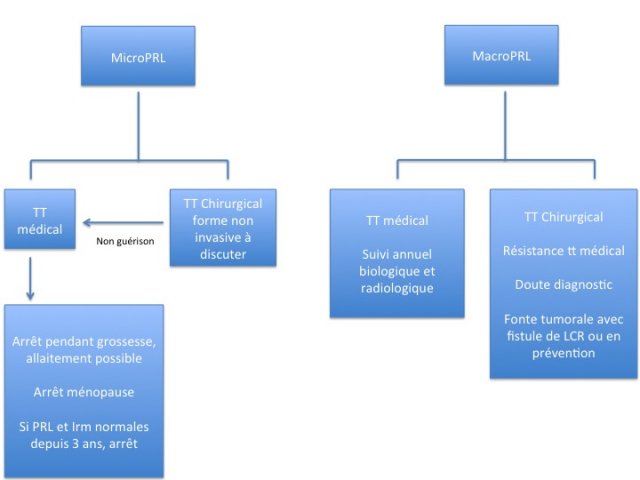
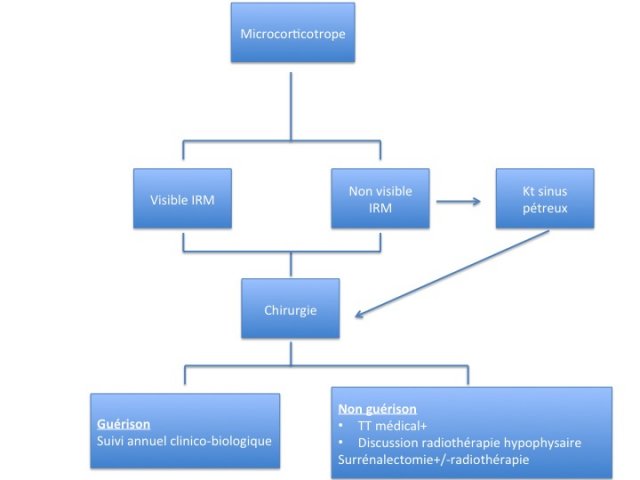
- Figures 14 : algorithme de prise en charge des prolactinomes, adénomes corticotropes et des adénomes hypophysaires non fonctionnels.
Somatotropic Adenomas
Failure of surgery or adenomas of average and small size with invasion of the cavernous sinus are indicated for medical treatment (management algorithm, Figure 4).

- Figure 4 : photos du syndrome dysmorphique de l’acromégalie. L’algorithme du bas résume la prise en charge actuelle de l’acromégalie où la priorité est donnée à la chirurgie autant que faire se peut.
![]() First-line treatment includes: First generation Somatostatin Analogues (SA) (Octreotide, lanreotide) acting on SST2 receptors that do exist on the membrane of the tumor cell in 90% of somatotropic adenomas) 16. These analogues suppress GH production thus decreasing cell volume and sometimes tumor volume. Their action is nevertheless cytostatic and by definition these analogues do not cure the patients. This treatment requires an IM or deep subcutaneous injection every 4 weeks. A first assessment (GH-IGF-1 +/- MRI) will be conducted on the eve of the 4th injection to evaluate tumor sensitivity to treatment and allow for adaptation of the regimen. An increase in the dose and / or an increase in the frequency of administration will be discussed if hypersecretion is not controlled.
First-line treatment includes: First generation Somatostatin Analogues (SA) (Octreotide, lanreotide) acting on SST2 receptors that do exist on the membrane of the tumor cell in 90% of somatotropic adenomas) 16. These analogues suppress GH production thus decreasing cell volume and sometimes tumor volume. Their action is nevertheless cytostatic and by definition these analogues do not cure the patients. This treatment requires an IM or deep subcutaneous injection every 4 weeks. A first assessment (GH-IGF-1 +/- MRI) will be conducted on the eve of the 4th injection to evaluate tumor sensitivity to treatment and allow for adaptation of the regimen. An increase in the dose and / or an increase in the frequency of administration will be discussed if hypersecretion is not controlled. ![]() The side effects of treatment are mainly gastrointestinal, from decreased secretion of pancreatic enzymes with malabsorption and diarrhea as well as gall stones. The use of pancreatic enzymes during SA injections can relieve patients and these digestive side effects decrease with time. Note of high cost of these treatments should also be taken into account.
The side effects of treatment are mainly gastrointestinal, from decreased secretion of pancreatic enzymes with malabsorption and diarrhea as well as gall stones. The use of pancreatic enzymes during SA injections can relieve patients and these digestive side effects decrease with time. Note of high cost of these treatments should also be taken into account.![]() Therapeutic efficiency correlates with the volume and hypersecretion with an average of 50% of responders at one year and 30% tumor volume reduction after this period. Although the therapeutic effect continues over time44, an inadequate response after 6 months of treatment should necessitate complementary treatment or change of therapeutic strategy.
Therapeutic efficiency correlates with the volume and hypersecretion with an average of 50% of responders at one year and 30% tumor volume reduction after this period. Although the therapeutic effect continues over time44, an inadequate response after 6 months of treatment should necessitate complementary treatment or change of therapeutic strategy.
The « criteria for control » are identical to « cure criteria » (mean GH <2.5 μg / l (7.5 ml / l), IGF1 normal for age, Nadir GH / OGTT <0,4μg / l (1, 2 ml / l)).
![]() Second line treatment include :
Second line treatment include :
- Dopamine Agonists: Their use in cases of mixed GH-PRL adenoma is apparent, but may be useful to treat « pure GH adenomas » because of the possible presence of dopamine receptors on cell membrane. They are used in combination with SA in case of uncontrolled disease, with moderate increase of IGF-1 (<1.3 times the normal) but may also be used as first line in moderate acromegaly.
- The new SA, pasireotide®, which is active on 4 of the 5 SST receptors is a second line therapeutic option and preliminary results show that it might be more effective in controlling hypersecretion and tumor volume and also in cases resistant to conventional SA 56.
- GH antagonist (fix and block liver GH receptors) or PEGVISOMANT®. Used in case of failure of the SA and allows the control in at least 70% of patients but has no anti-tumor effect. It is used as monotherapy in case of SA resistance or in combination with a SA in large tumors or severe manifestations of mass effect such as headaches (daily injection). IGF-1 levels only are done to monitor these patients in addition to regular liver function tests (baseline, day 15 and every 6 months) and an MRI at 6 months. Tumor volume increase has been described with the initiation of treatment or stopping the SA.
Corticotropic Adenoma
The therapeutic goal is to suppress corticotropic hypersecretion, even at the expense of an anterior pituitary insifficiency and treat complications.
In case of failed surgery, medical treatment will be implemented with the drug of choice being somatostatin analogues with an action on the pituitary: Pasireotide® (common side effects similar to those of SMS analogues with the risk of decompensation of diabetes) or anti-cortisol drugs with an adrenal action: OP’-DDD, Metopirone or ketonazole (an antifungal with risk of hepatitis). This treatment will be instituted pending a long lasting therapy that will be discussed on a case by case during Pituitary Multidisciplinary Meetings: pituitary redo surgery, bilateral adrenalectomy (sometimes associated with pituitary radiotherapy) or pituitary radiotherapy alone especially when the target has been well defined . In this case, medical treatment will be maintained during the period needed to obtain the effect of radiotherapy usually between 12 and 18 months.
The algorithm in figure 15 summarizes the strategy of the management of corticotropic microadenomas.
Thyrotropic Adenomas
Treatment can be surgical or medical (with somatostatin analogues) and aims to restore normal thyroid function.
Reported series in the literature involve small numbers of patients thus no definitive conclusions can be drawn.
SA are effective in controlling hypersecretion with 40% reduction in tumor volume because all thyrotropic adenomas strongly express subtype 2 and 5 receptors 16. SA are discussed as first line therapeutic option for average volume adenomas without visual affection even if there is lateral invasion.
Non-secreting or no-nfunctioning pituitary adenomas (gonadotrophin and "silent")
No medical treatment has demonstrated the long lasting effectiveness despite a few articles reporting results with dopamine agonists or somatostatin analogues 18,19.
The policy is in favor of surgery and is summarized by the algorithm in Figure 16.

Atypical Adenomas or Pituitary Carcinomas
Data on the use of Bevacizumab (Anti-angiogenic anti-VEGF (vascular endothelial growth factor)) and anti-mTOR is still rare36,54. Certainly, there is a pathophysiologic basis with overexpression of angiogenic factors and the activation of the PI3K / AKT / m-TOR pathway in some aggressive adenomas, but very few patients have currently been treated 33..
Pituitary Apoplexy
The treatment of pituitary apoplexy remains controversial and was the subject of a consensus meeting by the English society of Endocrinology60. Referral to a pituitary reference center is the rule. The controversy concerns the question "indication for surgery or conservative treatment" because literature is confusing without a randomized study. Schematically, patients considered for conservative treatment are those without severe or aggravating visual affection or disturbance of conscious level. Oculomotor palsies are not indications for surgery in the absence of problems with the visual field or acuity.
 Encyclopædia Neurochirurgica
Encyclopædia Neurochirurgica

