 Spontaneous intracerebral hemorrhages
Spontaneous intracerebral hemorrhages
Treatment options
The principles of treatment described below are from the 2010 recommendations of the American Heart Association and American Stroke Association (31).
*1 / Management.
In contrast to the current general attitude, the decision of therapeutic abstention and resuscitation should not be made until at least 48 hours of appropriate and intensive care. Given the absence of perfectly reliable predictive factors, any patient with SICH, even seemingly severe cases, should benefit from intensive care. However, this recommendation does not apply when the indication for non-resuscitative care is related to the patient’s past history (such as untreatable neoplasia, major organ failure ...) or a patient in a state of apparent brain death. Reevaluation is then necessary after 48H and the decision whether to continue or discontinue care should be taken during a multidisciplinary meeting.![]() The patient should be initially admitted in a neurovascular intensive care unit or even a neurointensive care with trained and competent personnel in the management of this pathology (I, B).
The patient should be initially admitted in a neurovascular intensive care unit or even a neurointensive care with trained and competent personnel in the management of this pathology (I, B).
*2 / Medical Treatment
a- A normal blood sugar should be maintained (insulinotherapy protocol) (I, C), and if possible hyperthermia should be avoided.
b-Antiepileptic treatment
Any symptomatic epileptic crisis should be treated and the treatment continued for several months (I, A). Prophylaxis is not indicated (III, B).
c- Blood Pressure Control
The current recommendations are:![]() If the systolic blood pressure (SBP) is greater than 200 mmHg or Mean Arterial Pressure (MAP) is greater than 150 mmHg, intravenous antihypertensive therapy (eg nicardipine IV) should be given rapidly and BP (blood pressure) be monitored every 5 minutes.
If the systolic blood pressure (SBP) is greater than 200 mmHg or Mean Arterial Pressure (MAP) is greater than 150 mmHg, intravenous antihypertensive therapy (eg nicardipine IV) should be given rapidly and BP (blood pressure) be monitored every 5 minutes.![]() If the SBP ≥ 180 mm Hg or MAP ≥ 130mmHg and there is a strong likelihood of increased intracranial pressure, it is advisable to monitor the intracranial pressure (ICP) and control the BP with IV antihypertensive drugs in order to maintain a cerebral perfusion pressure (CPP) ≥ 60 mmHg.
If the SBP ≥ 180 mm Hg or MAP ≥ 130mmHg and there is a strong likelihood of increased intracranial pressure, it is advisable to monitor the intracranial pressure (ICP) and control the BP with IV antihypertensive drugs in order to maintain a cerebral perfusion pressure (CPP) ≥ 60 mmHg.![]() If the SBP ≥ 180 mmHg or MAP ≥ 130mmHg without signs of intracranial hypertension, set up an IV antihypertensive treatment accompanied by clinical monitoring.
If the SBP ≥ 180 mmHg or MAP ≥ 130mmHg without signs of intracranial hypertension, set up an IV antihypertensive treatment accompanied by clinical monitoring.![]() In general, for patients with SBP between 150 and 220 mmHg, reducing it to around 140 mmHg, seems reasonable provided it is not deleterious on the CPP (IIa, B).
In general, for patients with SBP between 150 and 220 mmHg, reducing it to around 140 mmHg, seems reasonable provided it is not deleterious on the CPP (IIa, B).
d-Any patient with a deficiency in coagulation factors or thrombocytopenia should have a rapid correction of the deficit (I, C). Specific cases:
![]() Patients on vitamin K antagonist (VKA): This is a frequent occurrence (12-14% of SICH (36)), imposing specific measures: stop oral anticoagulant, immediate correction of the vitamin K dependent deficient coagulation factor by PPSB[Prothrombin-Proconvertin-Stuart Factor-Antihemophilic Factor B] (Kascadil for example) associated with a parenteral injection of vitamin K (with delayed effect) (I, C). The objective is to obtain an INR of 1.
Patients on vitamin K antagonist (VKA): This is a frequent occurrence (12-14% of SICH (36)), imposing specific measures: stop oral anticoagulant, immediate correction of the vitamin K dependent deficient coagulation factor by PPSB[Prothrombin-Proconvertin-Stuart Factor-Antihemophilic Factor B] (Kascadil for example) associated with a parenteral injection of vitamin K (with delayed effect) (I, C). The objective is to obtain an INR of 1.![]() Patients on antiplatelet agents: immediately stop the antiplatelet. The administration of platelets is not indicated, unless surgery is planned (IIb, B).
Patients on antiplatelet agents: immediately stop the antiplatelet. The administration of platelets is not indicated, unless surgery is planned (IIb, B).
e-Prevention of thromboembolic complications:![]() Stockings combined with intermittent pneumatic compression (I, B).
Stockings combined with intermittent pneumatic compression (I, B).![]() Preventive anticoagulation: it must be considered between D1 and D4 in a bedridden patient, provided there is evidence of cessation of bleeding (on control images) (IIb, B).
Preventive anticoagulation: it must be considered between D1 and D4 in a bedridden patient, provided there is evidence of cessation of bleeding (on control images) (IIb, B).
*3 / Neurosurgical Management
a-Intracranial Pressure (ICP) Monitoring
There is no data in the literature confirming the benefit of ICP monitoring in ICH in terms of functional outcome and mortality. The proposed indications are an extrapolation of the indications defined for head trauma. ICP Monitoring may be proposed in the following situations:
GCS ≤ 8, signs of temporal herniation (mass effect), hydrocephalus or IVH on the CT Scan (IIb, C).
The choice of using a fiberoptic ICP device or an External Ventricular Drain (EVD) depends on the situation. An ICP monitoring device with less complications should be preferred except in cases of hydrocephalus or IVH where only the EVD allows for an effective ICP control.
The ICP must be controlled so as to obtain a CPP between 50 and 70 mmHg.
b-Intraventricular Hemorrhage(IVH)
Occurring in approximately 45% of the cases with SICH, it constitutes a major factor for the severity of the ICH and is a subject for intense research (19). The current standard of treatment of IVH is EVD to control hydrocephalus. However EVD does not enable a rapid drainage of the IVH, and does not seem to improve the functional outcome (33). It was therefore proposed to inject via the EVD catheter a fibrinolytic agent (tPA or urokinase) to lyse the clot and thus accelerate the resolution of IVH. A recent meta-analysis of observational studies showed that intraventricular fibrinolysis (IVF) markedly decreased mortality and improved functional outcome, without increasing complications (13). However, no good quality randomized clinical trial has been so far published, and IVF cannot be strongly recommended, but its use decided upon on a case-by-case basis (IIa, B).
c- Surgical Treatment.
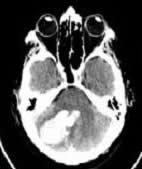
In most cases of ICH, surgical evacuation is not indicated (IIb, C). There are however some special cases:![]() Cerebellar ICH compressing the brainstem or causing obstructive hydrocephalus in a patient with neurologic deterioration. This indication is almost unquestionable (I, B) (Figure 7). EVD alone is not recommended.
Cerebellar ICH compressing the brainstem or causing obstructive hydrocephalus in a patient with neurologic deterioration. This indication is almost unquestionable (I, B) (Figure 7). EVD alone is not recommended.
![]() In case of supratentorial ICH, a recent meta-analysis on individual data suggests a benefit of surgery in the following situations (IIa, B) (18):
In case of supratentorial ICH, a recent meta-analysis on individual data suggests a benefit of surgery in the following situations (IIa, B) (18):
- Patients under age 69
- GCS between 8 and 12
- Hematoma volume between 20 and 50 ml
- No associated IVH
- Surgery performed within 8 hours of onset of symptoms
- ICH located less than a centimeter from the cortex (Figure 2).

- Figure 2: Left parietal-occipital lobar hematoma, suggestive of amyloid angiopathy in a hypertensive and / or aged patient. The cortical nature and its large volume is an indication for surgery.
The surgical procedure, which would not elaborated on here, must be performed under standard neurosurgical conditions, that is : by a conventional craniotomy. The authors recommend not to completely evacuate the hematoma (but at least 70%) in order to reduce the risk of rebleeding from the walls of the cavity. Currently, endoscopy or stereotactic techniques (associated or not with fibrinolytics) have not demonstrated their effectiveness and are under research (IIb, B).
*4 / Long-Term Management
a-Rehabilitation
Any patient with an ICH should be appropriately rehabilitated as soon as possible in a specialized center (IIa, B).
b-Prevention of recurrence
The prevention of recurrences is based on:![]() Treatment of arterial hypertension; the target blood pressure should be <140/90 mmHg (I, A). But it is likely that lowering of blood pressure is also beneficial in non-hypertensive subjects.
Treatment of arterial hypertension; the target blood pressure should be <140/90 mmHg (I, A). But it is likely that lowering of blood pressure is also beneficial in non-hypertensive subjects. ![]() Resumption of anticoagulants: it depends on their underlying indication and the topography of the ICH. In case of non-valvular atrial fibrillation at high risk of embolism, the resumption of VKAs may be considered if the ICH is deep (no argument for amyloid angiopathy) and if the predisposing factors for ICH (notably hypertension) are controlled (IIa, B).
Resumption of anticoagulants: it depends on their underlying indication and the topography of the ICH. In case of non-valvular atrial fibrillation at high risk of embolism, the resumption of VKAs may be considered if the ICH is deep (no argument for amyloid angiopathy) and if the predisposing factors for ICH (notably hypertension) are controlled (IIa, B).![]() Avoiding excessive alcohol abuse seems also to decrease the risk of recurrence (IIa, B).
Avoiding excessive alcohol abuse seems also to decrease the risk of recurrence (IIa, B).
 Encyclopædia Neurochirurgica
Encyclopædia Neurochirurgica

